The biology of menopause from a functional medicine perspective
Last month I watched with bated breath the BBC One documentary ‘The Truth about menopause’. Mariella Frostrup puts menopause front and centre and covers different approaches to dealing with symptoms such a diet, exercise, CBT and hormone therapy. At the Marion Gluck clinic we definitely agree with all of these approaches but believe they should all be used in unison as a holistic approach. I appreciate that our bodies are complex and optimising health works best when we really understand the biology of mind and body and the complexity of their interaction. Going back to basics, even us doctors, have long forgotten the biology of sex hormones and even for those of us who didn’t, it seems of little relevance as we look at disease with a ‘name it, shame it and tame it approach’, as we go about fixing things in one part of our bodies by giving a quick drug that suppresses one symptom as quickly as possible. And although this works in the acute medical model, in the chronic disease model it often gives side effects and risks. The benefits have to be carefully considered.
Moreover, with our desire and expectation for a quick fix/solution, we are often frustrated when the medical establishment does not deliver it. We approach ageing with fear and dread and usually overlook the process of conscious transformation that life entails, the wisdom and love that we could still be passing on as we age. Everything in our body is about balance and harmony. This is why I’d like to add to the conversation Mariella started by covering a bit more about the biology behind menopause as well as how all the hormones work together.
The revolution of fight or flight
Firstly, I want to acknowledge how much we women have achieved in the last hundred years, juggling childcare, from boardrooms to the trading floor, we wanted to have it all! Indeed we got it all, and we championed but sometimes I wonder how much we ended up actually doing and what impact this has had on our health and the transitioning process of menopause.
Our bodies have had to adapt accordingly. Humans among many other animals were designed to produce cortisol in short bursts to help us run away from danger – the fight or flight response. This is very different to how we operate now. Our busy modern lifestyles mean we are producing cortisol more frequently. Most people are aware of this but what most people don’t know is what is actually taking place in the body when cortisol is being constantly produced and how this affects our hormones. I believe it is really important to understand the steroid pathway, please stay with me on this one.
The Steroid Pathway
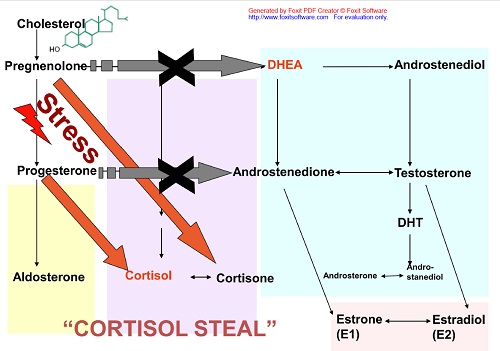
Take a moment to look at the chart and appreciate the little arrows that facilitate the ways our body can adjust hormones levels and balance them depending on what the perceived need is at any time point. As you can see from diagram 1, cholesterol is the first step in the process. We produce cholesterol first and this starts the production of all the other processes that produce our hormones. The main steroid hormones are pregnenolone, cortisol, progesterone, di-hydroepiandosterone (DHEA), testosterone and oestrogen (and several other metabolites in between).
Your body is completing these processes moment by moment. ALL.DAY.LONG!!
There are 2 ways our modern lifestyle and diet are affecting these processes:
- Diets that don’t include enough good fats
In order to produce cholesterol we need healthy fats in our diet. The western world has for many years encouraged a low fat diet and presented us low fat versions of everything (that have added sugar!). While there are bad fats to avoid, it is important to have healthy natural fats (avocados, nuts, seeds, oily fish, quality organic meat) as part of your diet. Our brain needs fat and so do our hormones.
- Chronic Stress – Cortisol is king
Cortisol is the ruler of hormones. When there is not enough cholesterol available to complete the steroid pathway the most likely scenario is that your body will only attempt to complete the cortisol pathway to manage the stress the body is under (diagram 1 – cortisol steal). Cortisol can also influence how we respond to oestrogen and progesterone. High levels of cortisol have been shown to make oestrogen and progesterone less effective (when you feel that the hormone therapy you are taking isn’t working for you, this may be a contributor). Cortisol may influence thyroid function and lead to symptoms of low thyroid. It can cause high insulin, insulin resistance and diminished ability to metabolise sugars, which in turn may cause weight gain (that extra tyre around our middle). To address high cortisol usually requires lifestyle changes. I believe that approaches like CBT, as in the documentary, may work by addressing cortisol.
Dietary changes that help include avoiding processed foods and refined sugars, to having more protein and quality fats at every meal, as well as incorporating mindfulness in our daily routines. Cortisol is the elephant in the room in our menopause conversations. If you want to understand stress, I recommend you order Dr Rangan Chatterjee’s upcoming book “The stress solution”, I trust him to deliver a down to earth approach that is rooted in the latest science.
Hormones dance together
If scientific diagrams don’t agree with you, we can think of hormones using a circle dancing analogy. You may remember dancing this way as a child. Do you remember what happened when the circle was broken? This could create a domino effect on both sides of the break. There are many interactions between various hormones and the brain and they all ‘dance’ together. This short film, Balance, by Wolfgang Lauenstein demonstrates the fine balance of our hormones perfectly and how they adapt to each other. If one is struggling, they all respond and adjust. Each tissue, however, has its limits in adjusting and balancing responses to our daily pressures. If there is an additional stress on the system, for example a bereavement or a conflict at work, cortisol production may increase. During times of stress, other pathways are diverted to favour cortisol production, e.g. pregnenolone and progesterone are converted to cortisol. Sustained stress may over time lower your DHEA levels and fatigue sets in.
Menopause as a takeover process
Coming back to the dancing analogy, at menopause, oestrogen and progesterone trip over and it can be a bit harder to keep the show on the road for a period of time.
My brief view of the biology of menopause is that menopause is, in essence, a takeover process. The ovarian function declines and the ovaries produce less oestrogen and progesterone. As women, we also make testosterone and dihydroepiandosterone (DHEA) and we continue to produce these from the adrenal glands after menopause. Our bodies have enzymes that transform testosterone into oestrogen and this is an important pathway for well-being once menopause sets in. So, after menopause we rely on adrenals for hormones and there is less flexibility in the system without the ovaries. The stress we take on in the preceding years may affect how well the takeover process unfolds.
Hormone therapy
Mariella’s hormone therapy was body-identical (bio-identical), meaning that the hormones she used have the same structure with what our bodies make (oestradiol and progesterone). Interestingly, using oestrogen alone as hormone therapy in earlier studies resulted in a decrease of breast cancer risk (but increased risk of uterine cancer, leading to incorporating progesterone-like drugs for hormone therapy. There are other synthetic progestins that are not progesterone and it is progestins that have been used in the clinical trials showing an increased risk of breast cancer. There isn’t enough data to confirm that using oestrogen and progesterone is safer with regards to cancer risk, however it makes sense to replace like for like if possible and to monitor levels to adjust dose, given that our metabolism slows down as we age.
The spectrum of hormone therapy available is wide. Some doctors remain reluctant to even offer it. For many women, Oestrogel (Oestradiol) and Utrogestan (Progesterone) is still not always available on the NHS and monitoring blood tests is currently not recommended by NICE. At the other end of the spectrum, bio-identical hormone therapy can use a more personalised approach and replace other hormones we naturally produce, such as testosterone and DHEA in addition to oestrogen and progesterone and may contribute to a more balanced system over all. Using dose adjustments and blood testing alongside lifestyle and psychological advice may help improve outcomes.
Bio-identical hormone prescriptions are made in compounding pharmacies and while not FDA approved, they are often registered, regulated and comply with the standards of the General Pharmaceutical Council (GPhC) and use materials and products approved by the Medicines and Healthcare Products Regulatory Agency (MHRA). Moreover, I increasingly find in my practice that some women who did not tolerate conventional HRT feel better on BHRT and those who add nutritional and lifestyle interventions often need much smaller doses of hormones to achieve optimal wellbeing and compounding preparations allow for this dose adjustment.
As a clinician, I know that when it comes to menopause it is not the hot flushes that we fear the most, but rather the changes to our brain and how it can at times feel like depression, dementia and ADHD all at once! And there is nothing more rewarding than to hear a woman saying that ‘I feel more like myself again’. I admit I loved it when the Dalai Lama said a few years back that ‘… women will save the world’, and I hope that our menopause conversations will bring us closer to ourselves and to each other.
Thank you to Mariella Frostrup for starting the conversation.
Also Read:
Adaptogens for Stress and Fatigue
Perimenopause signs & symptoms to expect
Menopause signs & symptoms to expect